Phimosis: meaning, symptoms and treatment
Co-author of the page: Dottor Roberto Miano Associate Professor in Urology at the Faculty of Medicine, University of Rome Tor Vergata.
Phimosis is a medical condition characterized by a narrowing of the foreskin, the skin covering the glans of the penis, that can cause difficulty or inability to uncover the glans. This disorder can manifest itself in various forms and degrees of severity, affecting the sexual health and general well-being of affected individuals.
Below, we will look in detail at what phimosis is, analyzing its anatomical description, associated symptoms, and the different treatment options available

What's on this page:
What it is phimosis
The term “phimosis” refers to a medical condition in which it is difficult or impossible to uncover the glans of the penis due to a narrowing of the foreskin.
Phimosis can affect sexual life and, in severe cases, sexual intercourse is not recommended because it could produce micro-trauma to the scarring, which in turn could worsen the condition of phimosis itself.
Under normal conditions, the foreskin easily retracts, allowing exposure of the glans and ensuring adequate hygiene and normal sexual function. However, when shrinkage of the foreskin occurs and the foreskin does not retract completely, this is referred to as phimosis. There is no hard data, but statistics state that between 2 and 4 percent of the male population has faced or faces this anatomical handicap.
Phimosis vs paraphimosis
Forcing the foreskin past the glans can generate skin tears resulting in further scarring or, in severe cases, can lead to paraphimosis, with the glans “choking.”
Paraphimosis occurs when the foreskin, once retracted behind the glans, cannot be returned to its original position. This situation can cause difficult blood circulation in the glans and lead to edema or potential complications if not treated promptly.
Diagnosis of phimosis
Diagnosis of phimosis typically involves a clinical evaluation by a professional such as a physician or urologist. During the physical examination, the clinician will carefully examine the foreskin and assess its ability to retract over the tip of the glans.
The diagnosis takes into account not only the ability to retract the foreskin, but also the presence of associated symptoms, such as irritation, inflammation, or recurrent infection in the genital area. Importantly, the diagnosis of phimosis is not necessarily followed by immediate intervention, and treatment will be tailored according to the severity of the condition and the symptoms present.
Penile phimosis: symptoms
Phimosis can manifest itself through several symptoms that reflect the shrinkage of the foreskin and any difficulties associated with its retraction. Common symptoms include the difficulty or inability to fully uncover the glans resulting in discomfort and pain. Individuals with phimosis also may experience discomfort during sexual intercourse and erectile dysfunction.

Phimosis can also predispose to skin irritation, inflammation or recurrent infections in the genital area, as difficulty in performing proper cleansing can promote bacterial growth.
The most common but not exclusive symptoms of phimosis may be:
- Penile pain
- Pain during sexual intercourse
- Erectile dysfunction
- Urinary retention
- Dysuria
- Skin ulcers
- Urethral itching
The diagnosis of phimosis is often made by the patient himself who notices the narrowing of the foreskin; however, it is always recommended to see a physician for evaluation of the case with a specialist examination.

Severity levels of phimosis
There are different stages of phimosis that can be classified according to the ability to retract the foreskin. In the medical field, a particular scale is used to define the levels of severity of phimosis: the Kikiros scale.
In this scale, 5 grades are identified to distinguish different pathological levels:
| Grade | Definition | |
|---|---|---|
| Not tight | Grade 1 | Total retraction but tightens at the base |
| Not tight | Grade 2 | Retraction but not below the glans |
| tight | Grade 3 | Partial retraction |
| tight | Grade 4 | Slight retraction |
| tight | Grade 5 | No retraction |
To simplify classification, there is a general tendency in common parlance to use only two terms: non-tight or tight phimosis.
Non-tight phimosis
Non-tight phimosis is the least severe form of phimosis and occurs when the foreskin can be retracted only partially and to a certain extent. In this condition, the foreskin may cause discomfort or difficulty during erection or cleaning of the penis. Generally, we speak of non-tightened phimosis for the first two grades on the Kikiros scale.
In this case, it is recommended to resolve the situation as soon as possible to avoid the possible occurrence of paraphimosis. If, for example, during sexual intercourse, the foreskin were to slide all the way to the base of the glans, the narrowest part of the foreskin could then become blocked just below the glans. This would prevent the skin from rising properly and would go on to create a constricting noose on the penis.
Paraphimosis requires urgent intervention aimed at preventing this situation from impeding blood flow from the glans

Tight phimosis
We speak of tight phimosis, the most severe case of phimosis, when the foreskin is so tight that it completely prevents the glans from coming out. This does not allow proper sanitation of the penis, creates difficulty in urination and prevents normal intercourse.
In the presence of tight phimosis, the glans may remain partially or totally covered by the foreskin, and the resulting anatomical handicap is evident. This condition becomes a problem that needs to be addressed urgently and with appropriate attention because it hinders some normal daily activities of the sufferer. On the Kikiros scale, tight phimosis characterizes the last 3 grades.
Phimosis: causes and types
What are the causes of phimosis? Phimosis can be classified into several categories, related to its physiological or acquired origin.
Congenital phimosis
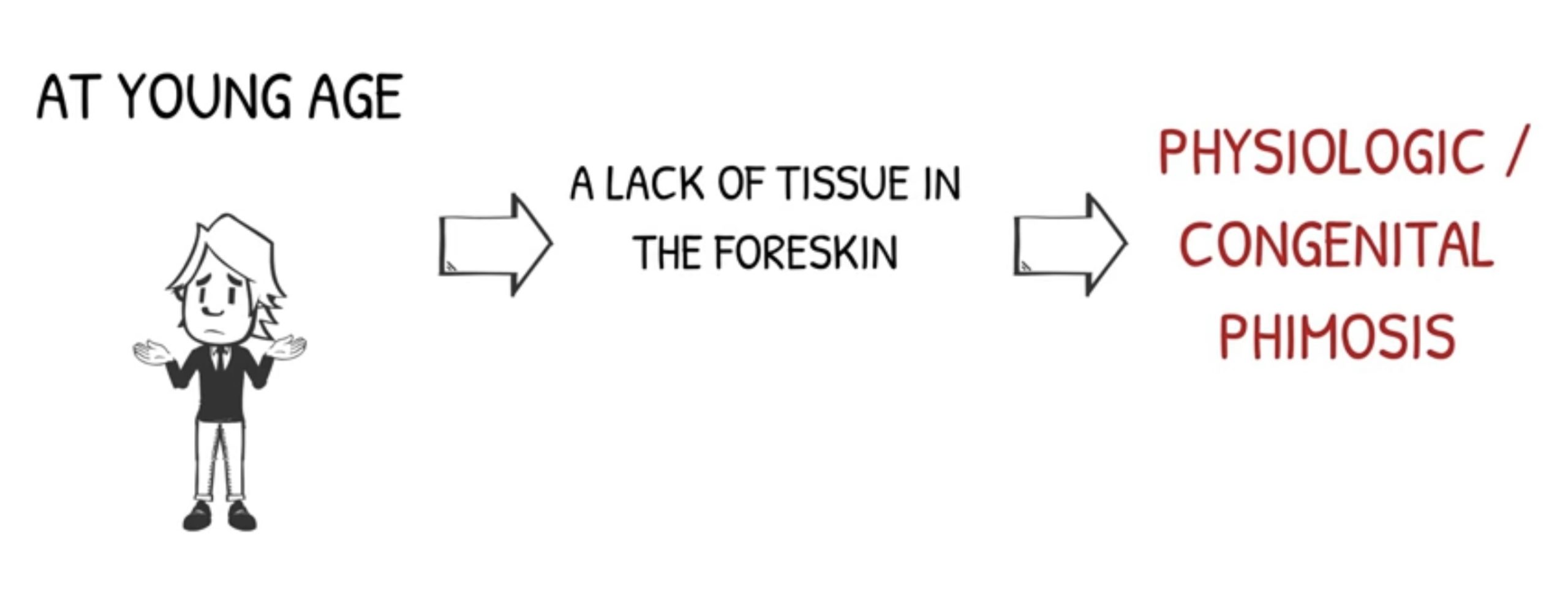
Congenital phimosis is present from birth, due to lack of elasticity of the foreskin, and in most cases is noticed in infancy/youth. It is a relatively common condition in infants and children, which tends to resolve on its own without the need for medical intervention.
At birth, male infants in fact have an abundance of preputial skin that hides the glans; this abundance, over time, adapts to the growth of the penis. Pediatricians advise, however, to check for tenacious adhesions between the inner part of the foreskin and the glans, preventing its uncovering.
In newborns, there is also shrinkage of the foreskin: this is a physiological shrinkage that is normally overcome with growth. In some cases, however, it happens that the foreskin does not enlarge along with the penis. This happens to about 1% of the male population and, as the years go by, creates an increasing difficulty in uncovering the glans. In this case it is called congenital phimosis.
If congenital phimosis is not tight, it might be noticed only at a young age, with the first spontaneous erections or in sexual activity. The shrinkage of the foreskin is so slight that it allows proper cleaning of the penis, but, during erection, prevents full uncovering of the glans. If, on the other hand, it is serratus phimosis, proper cleansing of the glans is also prevented and, on average, it is diagnosed before young age.
Some scientific studies state that the condition of phimosis in childhood is overdiagnosed because the physician does not distinguish between the natural non-retractability of the developing foreskin and a real pathological situation. Before recommending surgery, however, it would always be advisable to wait to confirm the diagnosis, since this condition can also be resolved in adulthood without surgery.
Acquired phimosis
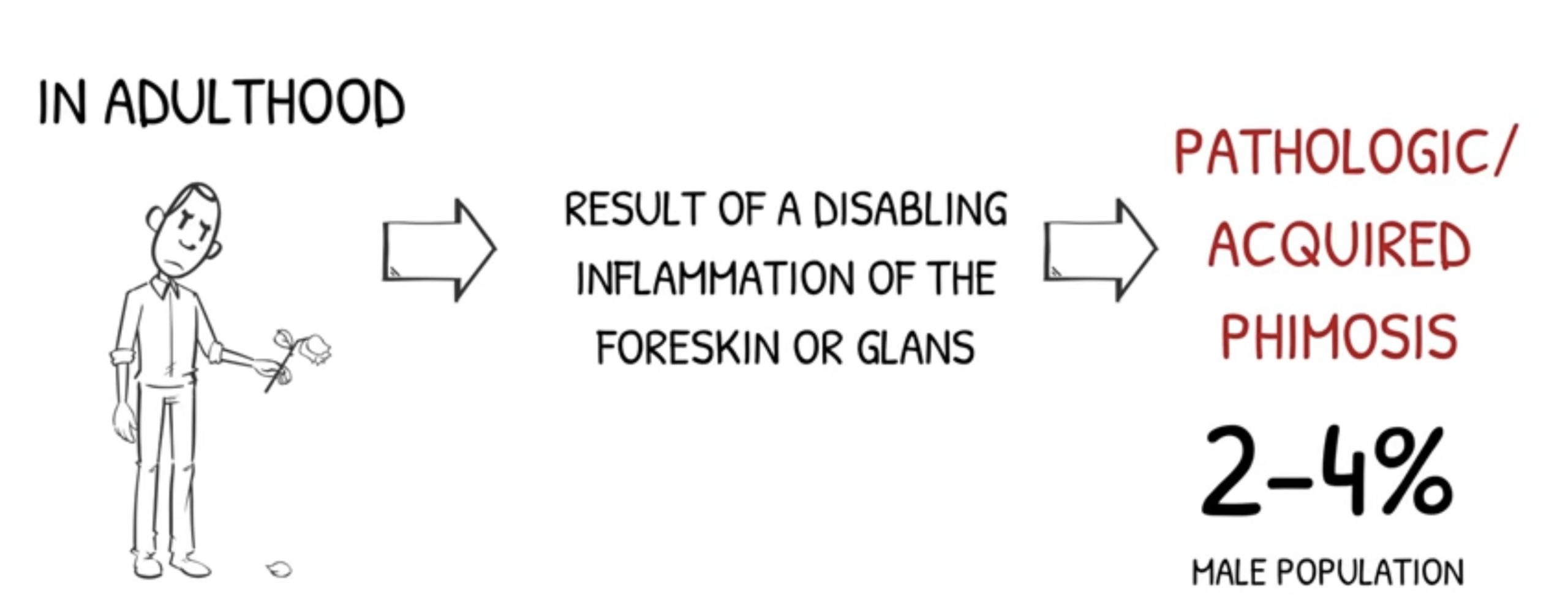
Acquired phimosis occurs in adulthood and is the disabling outcome of inflammation of the foreskin (balanoposthitis) caused by a microbial agent (bacteria and/or fungi).
Resolution of the infectious problem by medical therapy, however, often results in residual shrinkage and preputial scarring that is, indeed, referred to as phimosis. This, then, can cause thickening of the skin, making it less elastic and difficult to retract. In even simpler terms, here is what happens:
- Inflammation of the penis occurs.
- The inflammation is treated with appropriate medical therapy
- The treatment takes effect, but you see the formation of a “noose,” a circle of harder skin on the foreskin.
The “noose” that is formed is the phimotic ring, a collection of now inelastic epidermal cells. Scarring resulting from wound infection on the foreskin creates this ring, which, over time can become increasingly stiff, making it almost impossible to uncover the glans.
Complications
Phimosis is an anatomical handicap and cannot be called a disease or pathology. Possible complications arising from this medical condition are therefore all those pathologies that find an ideal state to arise in this situation.
There is therefore an increased risk of:
- Balanitis (inflammation or infection of the glans)
- Posthitis (inflammation or infection of the foreskin)
- Balanoposthitis (inflammation or infection of the glans and inner membrane of the foreskin)
The onset of these conditions may be due to the stagnation of smegma and urine in the penis, caused by phimosis and the inability to properly sanitize the part. If not properly treated, degeneration of such pathologies can lead to painful calcifications of the foreskin.
Prevention of phimosis
There is no way to prevent congenital phimosis, but in other cases it can be prevented through proper intimate hygiene.
In fact, prevention of phimosis often begins with proper hygiene practices, especially in the early years of life. Proper washing of the penis can help maintain cleanliness in the genital area and can be helpful in preventing problems related to phimosis. In addition, forced manipulation of the foreskin should be avoided, as such actions can cause trauma and scarring that could contribute to skin tightening.
A healthy lifestyle, including good hygiene and timely medical advice in case of suspicious symptoms, can contribute significantly to the prevention of phimosis. Importantly, although some forms of phimosis are normal during childhood and tend to resolve as the child grows, vigilance and attention from medical professionals are crucial to identify and manage any cases that require more specific interventions.

Phimosis treatments
Therapies to treat phimosis depend on the severity of the condition and associated symptoms.
Treating phimosis at a young age
On the treatment of congenital phimosis in youth there are different schools of thought among pediatricians. In some cases, appropriate exercises that allow the foreskin to regain its elasticity are recommended. Such exercises must, however, be done very carefully and cautiously to avoid going to worsen the situation. In other cases, appropriate therapy with steroid ointments is recommended.
The use of creams with steroids, in congenital phimosis in youth, can lead to the solution of the case without trauma. The important thing is to always follow the instructions of one’s medical professional, never forcing the situation. Especially for younger patients, there now seems to be a widespread idea among physicians to avoid circumcision unless strictly necessary. This assumption has also been confirmed by positions taken by the APA American Academy of Pediatrics.

Treating phimosis in adulthood with Phimostop
In most cases, to treat phimosis in adults, doctors tend to recommend circumcision with local anesthesia. While surgery is certainly a definitive solution, it does not take into account the psychological and human implications that the patient must face before deciding to have part of his penis removed.
For this reason, it is important to propose alternative avenues before arriving at surgical treatment. Phimostop is the only medical device designed to treat phimosis without circumcision surgery, thanks to 22 medical silicone elements. The latter are designed to elasticize the phimotic ring through the well-established technique of skin dilation when subjected to progressive and constant pressure.
Source:
- https://www.nhs.uk/conditions/phimosis/https://www.sciencedirect.com/science/article/abs/pii/S0090429519309197
- https://www.chop.edu/conditions-diseases/phimosis
- https://urology.ucsf.edu/patient-care/children/phimosis